An update to this article has been published. To view it, click here : https://www.healtis.com/en/orthopedic-devices-how-to-assess-safety-in-mri-update-12-12-24/
MRI is one of the most demanding electromagnetic environments.
For medical devices made of metallic, magnetic or electrically conductive materials, exposure to MRI can give rise to risks that need to be assessed to gain access to major markets.
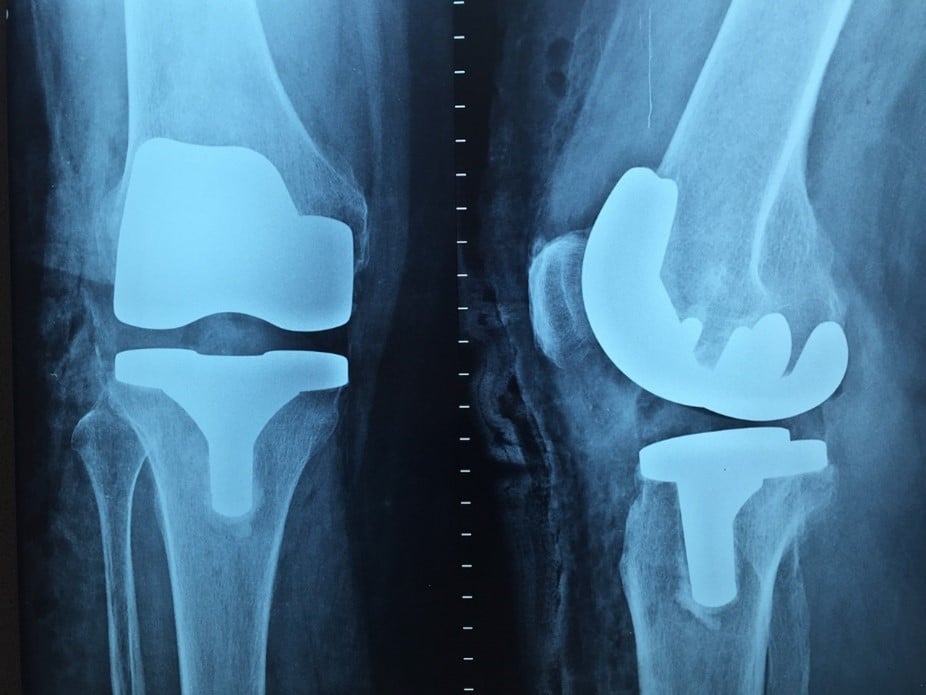
What about implantable or semi-implantable orthopedic systems?
It has become mandatory to assess the MRI safety of orthopedic devices in major markets, particularly the United States and Europe.
What tests must be carried out on orthopedic implant systems?
The vast majority of orthopedic systems are made of conductive materials (titanium, cobalt-chromium, stainless steel, etc.). When such a device is introduced into the MRI, several effects are produced, including an attractive force and torque induced by the MRI’s magnetic field, and heating due to the radiofrequencies present during the examination. Image disturbance (“artifacts”) is also observed in the vicinity of the device.
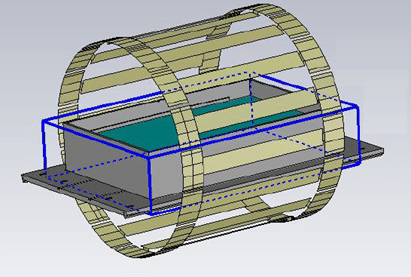
These effects are potential risks that need to be assessed. This assessment generally requires testing to ASTM standards (ASTM F2052, ASTM F2213, ASTM F2182 and ASTM F2119).
These tests are carried out on “worst-case” configurations. For magnetically induced force and torque on your device, as well as for artifacts, these worst-cases are, in general, easily identifiable, and a discussion with our team is usually all that’s needed to clarify the matter.
As far as radiofrequency heating is concerned, the variability of clinical configurations makes worst-case prediction complex, if not impossible, without in-depth study.
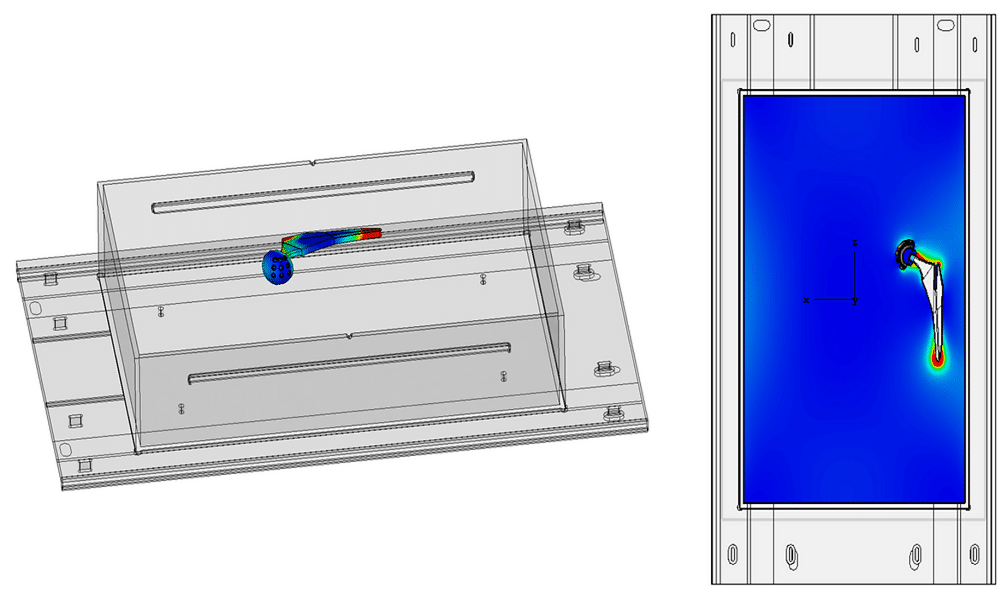
For a given range of orthopedic implants, it is therefore necessary to research the worst-case configuration using numerical simulations.
Focus on the use of numerical simulation to determine the worstcase configuration
At Healtis, we offer a numerical simulation service that makes it possible to identify a worst-case configuration: the configuration that will heat up the most among the many possible clinical configurations.
These simulations can also be used to identify hot spots on the device, which will then be monitored when this worst-case configuration is tested in MRI.
To conclude
For orthopedic systems (knees, hips, shoulders, etc.), the main difficulty in MRI risk assessment is generally determining the worst-cases for assessing radiofrequency-induced heating.
Simulation proves to be an effective and precise tool for optimizing this research. The number of configurations to be simulated will depend on the characteristics of the device and the rigor with which the manufacturer wishes to determine his worst-cases. Please contact us to discuss this further.
It should also be noted that the assessment of heating carried out under the conditions defined by ASTM F2182 may not be sufficient to correctly estimate the expected in vivo temperature. An additional step is often required to extrapolate test results and better estimate expected heating in humans.
Any questions about this assessment? Contact us now at [email protected] !